PCOS, which affects around 116 million women globally, is recognized as the most prevalent endocrine disorder among women in their reproductive years.
To gain a deeper understanding, let’s delve into the definitions of PCOS and autoimmune diseases, explore their shared characteristics, and examine the connections between PCOS and established autoimmune conditions. This will provide a guide for us to head on to give a detailed answer based on the risen question, “IS PCOS AN AUTOIMMUNE DISEASE”
Additionally, we’ll explore various treatment approaches for autoimmune diseases and emphasize the significance of seeking medical attention to effectively manage PCOS symptoms and minimize potential complications.
WHAT IS PCOS?
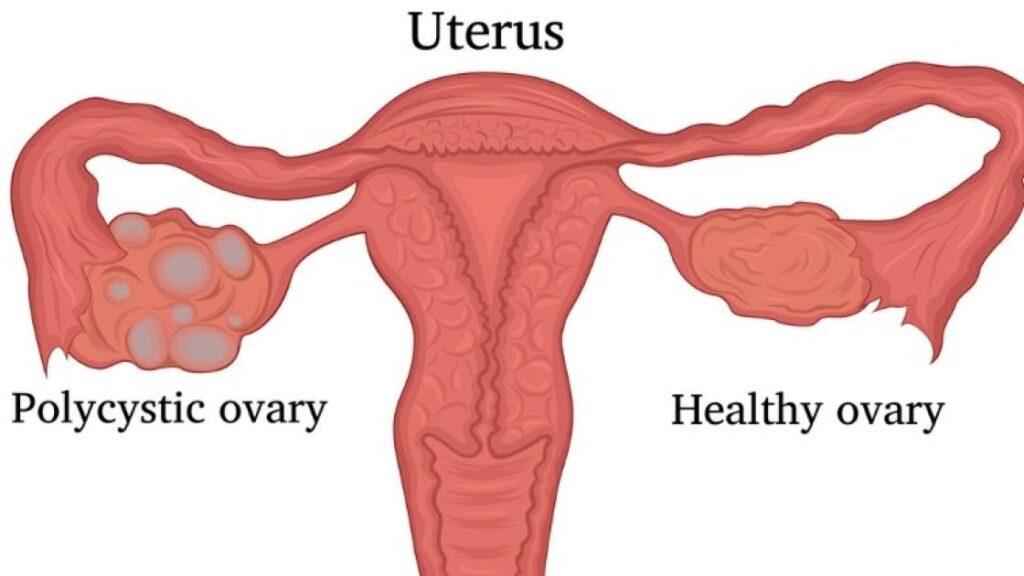
PCOS (polycystic ovary syndrome), affecting over 10% of women in their reproductive years, stands as the most prevalent endocrine disorder among women. This condition arises when a woman produces an abnormal amount of male sex hormones, often associated with the formation of small cysts in the ovaries, from which it derives its name. However, it’s important to note that some women with PCOS experience symptoms despite the absence of cysts.
Many women become aware of their PCOS diagnosis during their 20s and 30s when they embark on the journey of conceiving a child. PCOS can pose challenges to fertility, although it can manifest at any time following puberty. Among the array of symptoms associated with PCOS, irregular menstrual cycles, weight gain, and hair thinning are a few noteworthy examples.
WHAT IS AN AUTOIMMUNE DISEASE?
The medical community recognizes over 80 distinct types of autoimmune diseases. In these conditions, the body’s immune system produces antibodies that mistakenly attack its own healthy cells instead of targeting bacteria and viruses, which they are designed to combat.
Autoimmune diseases pose unique challenges due to the intricate nature of the immune system and its complex interactions. Moreover, these conditions often persist throughout a person’s lifetime.
When you encounter a common cold, your immune system eventually triumphs over the infection. However, in the case of autoimmune diseases, the immune system remains engaged in a continuous battle against the body’s own cells. As a result, the damaged cells are replaced by healthy ones, perpetuating the autoimmune reaction and leading to the persistence of symptoms over the long term.
SIMILARITIES BETWEEN PCOS AND AUTOIMMUNE DISEASE
Like many autoimmune diseases, the precise cause of PCOS remains unclear. However, certain lifestyle factors, such as an unhealthy diet, excessive stress levels, and inadequate rest and sleep, are believed to contribute to the development of PCOS, much like other autoimmune conditions. If you find yourself leading a high-stress lifestyle, neglecting self-care, and experiencing disruptions in your menstrual cycle, it may be prudent to reconsider your priorities and make necessary changes to promote your overall well-being.
Presence of Autoantibodies
Adopting a functional medicine viewpoint, there are notable similarities in the underlying root causes of PCOS and autoimmune diseases. Both conditions exhibit a connection with the presence of autoantibodies, such as antinuclear antibodies and anti-thyroid antibodies, which suggest the involvement of autoimmunity. Autoantibodies serve as significant indicators of autoimmune diseases, as they recognize the body’s own tissues as targets and trigger the immune system to initiate attacks. However, it is important to note that autoantibodies can also be present in healthy individuals, particularly as they age. Consequently, the presence of autoantibodies alone is not sufficient for the diagnosis of autoimmune diseases. Additional factors and diagnostic criteria need to be considered to reach a conclusive diagnosis.
Insulin resistance
Furthermore, insulin resistance serves as a common risk factor for the development of PCOS, and it is also observed in various autoimmune disorders like rheumatoid arthritis and systemic lupus erythematosus (SLE).
Insulin resistance occurs at the cellular level and leads to an excess of insulin in the bloodstream. Insulin plays a crucial role in regulating blood sugar levels by facilitating the storage of sugar in cells as fat. When insulin resistance develops, cells become less responsive to the hormone, resulting in the inability to efficiently convert the sugar in the bloodstream into energy stored within cells.
In the case of PCOS, elevated insulin levels contribute to the production of androgenic hormones, disrupting the ovulation process and giving rise to many PCOS symptoms. In autoimmune diseases, increased systemic inflammation can contribute to insulin resistance. There even exists a rare autoimmune disease known as type B insulin resistance, which is characterized by the presence of anti-insulin receptor antibodies leading to insulin resistance at the cellular level.
While the exact mechanisms driving insulin resistance in PCOS are not yet fully understood, it is plausible that an autoimmune reaction within the body may be a causative factor for some individuals. The intricate relationship between PCOS, insulin resistance, and autoimmune processes requires further exploration and investigation to unravel the precise connections and underlying mechanisms involved.
Low-grade systemic inflammation
Research has indicated that women with PCOS have a higher likelihood of experiencing low-grade systemic inflammation. Inflammation is a normal response triggered to aid in the healing process and act as the body’s initial defense against infections. However, in certain individuals, the immune system remains persistently activated, leading to ongoing damage and disruption of other hormonal functions within the body. This immune activation can contribute to the overproduction of androgens from the polycystic ovaries.
In the case of autoimmune diseases, emerging evidence suggests that an aberrant inflammatory response may serve as an underlying cause for conditions such as inflammatory bowel disease, rheumatoid arthritis, and SLE.
Considering the significant role played by systemic inflammation in both PCOS and autoimmune diseases, it is plausible that the root cause of this inflammation, such as an imbalance in the gut microbiome, a high viral load, exposure to toxins, or chronic life stress, could potentially be a contributing factor in both conditions. Understanding and addressing these underlying factors could prove valuable in managing the inflammatory response and improving symptoms in individuals affected by PCOS and autoimmune diseases.
IS PCOS AN AUTOIMMUNE DISEASE
Presently, No!
While there are notable connections between PCOS and autoimmune diseases, it is important to note that PCOS is currently classified as an endocrinopathy or a disorder of the endocrine system, rather than an autoimmune disease. The distinction lies in the primary focus of PCOS being an hormonal imbalances and their effects on reproductive health, whereas autoimmune diseases involve the immune system mistakenly attacks the body’s own healthy cells and tissues.
METFORMIN FOR PCOS
Metformin is a medication commonly prescribed for the management of polycystic ovarian syndrome (PCOS). It is primarily used to treat type 2 diabetes, but it can also be beneficial for women with PCOS, particularly those who have insulin resistance or glucose intolerance.
Metformin works by reducing insulin resistance, improving insulin sensitivity, and lowering glucose production in the liver. In women with PCOS, insulin resistance is a common feature that can contribute to hormonal imbalances, irregular menstrual cycles, difficulty in ovulation, and other symptoms.
The use of metformin in PCOS aims to address insulin resistance and its associated effects. By improving insulin sensitivity, metformin can help regulate menstrual cycles, promote ovulation, reduce androgen levels (male hormones), and potentially improve fertility outcomes. It may also have additional benefits such as aiding in weight loss and improving lipid profiles.
It’s important to note that metformin is typically not recommended as a standalone treatment for PCOS but is often prescribed in conjunction with lifestyle modifications such as a healthy diet and regular exercise. These lifestyle changes, coupled with metformin, can yield better results in managing PCOS symptoms.
While metformin can be effective for many women with PCOS, it may not be suitable or necessary for everyone. It is important to have a thorough evaluation and discussion with a healthcare professional to determine the most appropriate treatment approach for your specific situation.
Overall, metformin can be a valuable tool in managing PCOS, particularly in cases where insulin resistance is present. However, it is just one component of a comprehensive treatment plan that may include lifestyle changes, other medications, and targeted interventions tailored to individual needs.
HOW TO CURE PCOS PERMANENTLY
Polycystic ovarian syndrome (PCOS) is a chronic condition that currently does not have a known cure. However. Various approaches to managing PCOS and reducing its symptoms effectively include:
Lifestyle modifications: Making positive changes in your lifestyle can have a significant impact on managing PCOS. This includes maintaining a balanced and nutritious diet, engaging in regular physical activity, managing stress levels, and ensuring sufficient sleep.
Weight management: If you are overweight or obese, losing even a modest amount of weight (around 5-10% of your body weight) can help improve hormonal balance and alleviate PCOS symptoms. A combination of healthy eating, portion control, and regular exercise is recommended.
Medications: Depending on your specific symptoms and health goals, your healthcare provider may prescribe medications to address specific concerns associated with PCOS. This may include hormonal birth control to regulate menstrual cycles, anti-androgen medications to manage excess hair growth or acne, and medications to promote ovulation for those trying to conceive.
Fertility treatments: For women with PCOS experiencing difficulties in getting pregnant, fertility treatments such as ovulation induction or assisted reproductive technologies like in vitro fertilization (IVF) may be recommended.
Managing specific symptoms: Individual PCOS symptoms such as acne, excessive hair growth (hirsutism), or hair loss may be addressed through targeted treatments such as topical creams, laser hair removal, or medications designed to manage these specific concerns.
CONCLUSION
On the whole, while PCOS shares some similarities with autoimmune conditions, it is recognized as a distinct endocrine disorder within the medical community.
FREQUENTLY ASKED QUESTON
IS FIBROMYALGIA AN AUTOIMMUNE DISEASE
The classification of fibromyalgia as an autoimmune disease is a topic of ongoing debate and research within the medical community. Fibromyalgia is a complex chronic pain condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and other symptoms.
While fibromyalgia shares some similarities with autoimmune diseases, such as chronic pain and fatigue, it does not fulfill the criteria required for classification as an autoimmune disorder. Fibromyalgia is currently understood to be a disorder of central nervous system processing, involving abnormalities in pain perception and processing.
REFERENCES
V. J. Hamilton “Is polycystic ovary syndrome an autoimmune disease? 2022
